Atrial Fibrillation Tutorial
Westby G. Fisher, MD, FACC
Director, Cardiac Electrophysiology
Evanston Northwestern Healthcare, Evanston, IL, USA
(Last updated 13 Mar 2007)
INTRODUCTION
So your doctor tells you you have atrial fibrillation. A myriad of questions circle through your head: What is atrial fibrillation? Where did it come from? Why do I need to be on warfarin (Coumadin®)? What options are there for treating this heart rhythm disorder? Will a pacemaker correct or control this rhythm. Do I need a surgical procedure? My doctor mentioned I also have atrial flutter; how is this different from atrial fibrillation? Etc., etc.
After treating many patients with atrial fibrillation, I can tell you that there is only one thing that is true: everybody's a bit different: different in how they perceive their atrial fibrillation, different in how they respond to medications, and different in what I recommend to them regarding therapy. This tutorial is basically what I tell patients in my practice about atrial fibrillation. I find it often takes an hour or so to explain the intricacies of the disease, and many leave forgetting much of the information that I told them. So I decided to produce this series of webpages to serve as a reminder of our conversation, and to serve as a reference for others. More and more I find patients bringing me articles they found on the internet, and so, with a bit of reluctance, I am contributing a bit to the worldwide web. Although references will be attached, I find that all the articles and resources can be confusing for the patient, so I'll try to avoid too many big medical terms in favor of distilling the important information that I find my patients asking. The information contained here is supplied free of charge. As such, each person should not use this information as their sole resource or recommendation for their care: you still need to seek care with your primary physician, cardiologist, or cardiac electrophysiologist (a heart rhythm specialist) and work with them to assure the proper care for your atrial fibrillation.
How Does the Heart Beat Normally? To understand how atrial fibrillation causes problems for you, you must first understand how the heart beats normally.
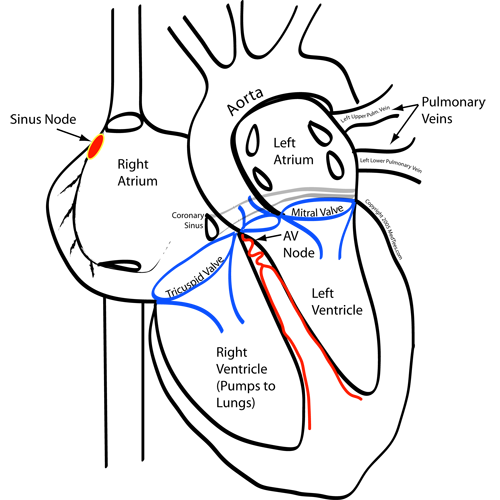
- The Normal Heart Beat. The human heart has four chambers, the upper two chambers are called the right atrium and left atrium, and the bottom two chambers are called the right ventricle and left ventricle (Figure below). The atrial chambers receive blood from various parts of the body, whereas the ventricles deliver blood (through vigorous pumping) to various organs of the body (the right ventricle delivers blood just to the lungs, where the left ventricle delivers blood to the rest of the body). As such, the atria can be thought of as holding areas for blood before it is deposited in the ventricles. The atria are important for "priming " the pumping chambers, that is, they perform the important function of filling the ventricles with the final bit of blood before it is ejected out to the rest of the body by the ventricules to improve the efficiency of their pumping action.
- All cells of the heart (except the heart valves) can beat rhythmically on their own if supplied with the right amount of oxygen and nutrients to permit proper function. This beating is caused by a small amount of charged salt ions that move across a cell's membrane wall very rapidly (similar to creating a small "spark" in a gas engine), which stimulates the cell's movement mechanism to contract. Some cells naturally beat faster than others (typically atrial cells beat faster than ventricular cells). Because the cells are all interconnected, the spark from one cell moves to the next cell, stimulating it, and this is passed to the next cell and so on. Therefore, the fastest beating cells cause the other cells next to them to contract, thereby driving the heart rate up to that of the fastest beating cells. Normally, there is a normal smooth sequential electrical activation of cells from a pacemaker group of cells in the upper right atrium (called the sinus node) that spreads evenly and uniformly across the upper two atrial chambers very rapidly (from one side to the other in about 50-100 thousandths of a second!), but this electrical wavefront cannot pass to the lower chambers because they are insulated from the upper chambers by the fibrous heart valves that separate the upper from lower chambers, except in one spot called the "AV node."
- Between the atria and ventricles there is a small specialized group of cells that serve as the only electrical connection between the atria and ventricles called the atrioventricular node or "AV node," for short. The AV node serves the important function of slowing the electrical conduction from the atria to the ventricles. This slowing provides time for the heart to move blood from the upper chambers (the atria) to the lower chambers (the ventricles). It is the AV node that is the target for many of the medications used to control the heart rate in patients with rapid heart rhythms or some surgical corrections of atrial fibrillation (more on this later). After the electrical wavefront of a heartbeat passes through the AV node, it spreads rapidly throughout the ventricular conduction system, causing the right and left ventricles to contract quickly, delivering blood from the heart chamber to the organs they supply.
So What is Atrial Fibrillation?
Atrial fibrillation is an irratic rhythm that occurs within the upper chambers of the heart (the "atria"). All of us have cells that occasionally beat out of sequence from the normal activation. If these skipped beats occur rapidly in succession, they can cause the cells in the atria to no longer activate in a smooth, uniform, and sequential fashion, and instead activate rapidly and chaotically, creating a series of rapidly circulating wavelets of activation, resulting in all the cells of the atria activating between 250 and 500 times per minute. The atrial chambers quiver when this occurs and no longer pump blood efficiently, permitting blood to pool within the atrial chamber, and on occasion, clot. When this happens, small portions of clotted blood can shower from the atrium and cause occlusion of blood vessels, even in the brain, and thereby cause a stroke to occur. In fact, it is estimated that 15% of all strokes are caused by atrial fibrillation. It is this reason that doctors have recognized the importance of anticoagulation at stroke reduction.
Where Does Atrial Fibrillation Come From?
In studies of catheter ablation of atrial arrhythmias, it was discovered that the initiating beats that cause atrial fibrillation often arise within the pulmonary veins that bring oxygenated blood back from the lungs to the left atrium (Haissaguerre, et.al,, New Engl J Med, 1998; 339(10) , Chen SA, et al ,Circulation, 1999 Nov 2; 100(18): 1879-86, and Jais P, et.a.l., Circulation 1997; 95: 572-576). The pulmonary veins attach to the left atrium which is just upstream from the left ventricle (the chamber that supplied blood to the majority of the body and brain). As such, procedures involving the pulmonary veins must be performed when the patient is anticoagulated to avoid clots from forming on the instruments used (which also could migrate to the brain and cause a stroke). In some cases it was noted that rapid rhythms caused by these cells caused the atria to beat erratically. More recently, data has evolved that suggests this simple concept probably does not account for many of the mechanisms of the initiation of atrial fibrillation. Newer data suggests the cells around the pulmonary veins which are richly innervated by the nervous system might also play a role in the initiation and, perhaps, the maintenance of atrial fibrillation (Pappone C, et al., Circulation 2004 Jan 27; 109(3): 327-334). In fact, there are data to suggest that wider-area ablation around the pulmonary veins has slightly improved outcomes than selective electrical isolation of individual pulmonary veins (Oral H, et al., Circulation 2003 Nov 11, 108: 2355). Nademanee et al (Nademanee K, et al, "A New Approach for Catheter Ablation of Atrial Fibrillation: Mapping of the Electrophysiologic Substrate," J Am Coll Cardiol 2004; 43: 2004-2053) later discovered that burning irregular signal locations in the atrium itself (so called "fractionated electrograms") could also achieve fairly high success rates with cahteter ablation. Therefore, the approach to catheter-based treatments of atrial fibrillation will vary from institution to institution, depending on the treating electrophysiologist's bias in this regard. Remember, as of the date of this article, no prospective, randomized trial comparing treatment strategies exists.
What Are My Therapeutic Options? The appropriate therapy probably is based first and foremost on your symptoms. First of all, ALL patients with atrial fibrillation should receive some form of anticoagulation. Patients with (a) structurally normal hearts as determined by echocardiography and (b) no associated risk factors, might be treated with aspirin alone. Risk factors identified with stroke risk include: (1) age equal to or greater than 75, (2) diabetes, (3) history of hypertension, (4) prior stroke, or (5) history of a weakened heart muscle or narrowing of the mitral valve (the valve between the left atrium and left ventricle). Patients in these categories, or with a structurally abnormal heart for any reason, should probably be treated with the blood thinner warfarin (Coumadin®) therapy.
The treatment strategies are generally based on three sets of symptoms: patients with (1) FAST/IRREGULAR rhythms, (2) SLOW, symptomatic rhythms, or NO SYMPTOMS.
- For patients with symptoms of FAST, irregular heart rhythms during periods of atrial fibrillation, whether this is felt or not (continuous rapid beating of the heart can cause the heart muscle to become weakened) the following therapies exist:
- Medication - Anticoagulation plus one of two different forms of medications:
- Rate-control medications (digoxin, beta-blockers (metoprolol, atenolol, inderal, carvedilol, etc.), or calcium channel blockers (diltiazem, verapamil)). These drugs just control the heart rate during periods of atrial fibrillation and are not known to necessarily convert atrial fibrillation back to normal rhythm.
- Rhythm control medications (the antiarrhythmic medications including flecanide, sotalol, propafenone, dofetilide, or amiodarone). These drugs are used to maintain normal rhythm or to convert the rhythm from atrial fibrillation back to normal rhythm. These drugs have considerably more side effects than rate control drugs and are at best 50-60% effective at preventing episodes of atrial fibrillation. Because of this relatively poor efficacy rate, anticoagulation is recommended to continue, even while on these medications, to reduce the risk of stroke.
- Cardioversion - This is where an external brief but powerful shock is applied to the chest to restore the atrial fibrillation back to normal rhythm. This is usually done as a same-day procedure where you come in the hospital briefly to be put to sleep, then a large shock is applied to your chest to restore the heart rhythm to normal. It should be noted that after one year, approximately 90 percent of patients will have a recurrence of atrial fibrillation, despite undergoing this procedure. Nonetheless, if your episodes of atrial fibrillation are infrequent (such as annually or so), this still might be an acceptable form of therapy. Additionally, if you are one of those lucky 10% of patients in who sinus rhythm is maintained, it is a simple, reasonably low-risk procedure to undergo.
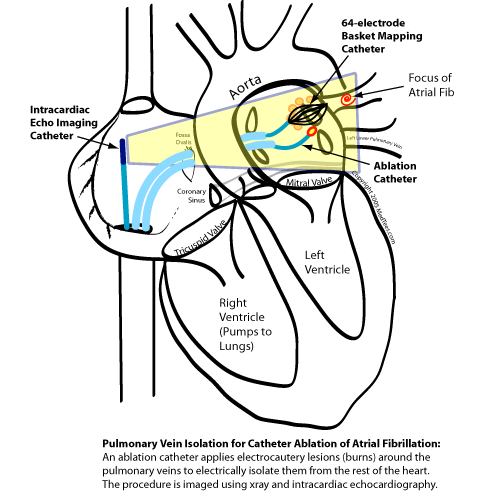
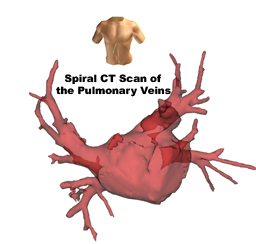
- Catheter Ablation of the initiating focus of atrial fibrillation (pulmonary vein isolation) - In this case, a series of wires called "catheters" are passed under local anesthesia into the heart from the blood vessels in your legs and small electrocautery burns are placed around the opening of the pulmonary veins into the left atrium. By burning around the openings of the pulmonary veins, these veins are electrically "disconnected" from the rest of the left atrium, and abnormally-firing cells in the pulmonary veins can no longer disturb the normal cells in the atrium. Because the procedure requires crossing from the right atrium to the left atrium by making a small puncture in the wall between these chambers, it is performed by specialized centers experienced in this technique. It therefore involves more procedural risks than other procedures to treat atrial fibrillation and is performed by a skilled cardiac electrophysiologist (a doctor specialized in the treatment of heart rhythm disorders). Procedures often take 3-5 hours to perform. The procedure is typically preceded by obtaining a special "spiral" CT scan (see image below) or MRI that serves two purposes: (1) to plan the procedure (evaluate the size and number of pulmonary veins and (2) to serve as a baseline for evaluation of pulmonary vein narrowing on follow-up CT scans late after the procedure. Occasionally, some centers require a transesophageal echocardiogram (a procedure that requires intravenous sedation so a probe can be placed in the swallowing tube (esophagus) behind your heart to acquire high-resolution images of the left atrium) be performed to assure no visible thrombus exists within the left atrium before proceeding with catheter ablation. The largest risks with this procedure include stroke (<=1%), cardiac perforation (<=1%) and late narrowing of the opening of one or more pulmonary veins (also called pulmonary vein stenosis) in <=1% of cases. If late pulmonary vein stenosis occurs (and again, clinically significant narrowing is uncommon), then the condition can result in long-term shortness of breath, disability, possible chronic cough, and rarely coughing up blood. Rare cases of death or serious infection caused by a hole in the heart that communicates with the esophagus (swallowing tube behind the heart) have been reported (Pappone C, et al., Circulation 2004 May 24; 109: 2724-2726), but are very rare (2 cases in 4360 patients) and thought to be caused by aggressive burning of the areas on the back wall of the heart. A comprehensive self-reported survey of 181 centers performing atrial fibrillation between 1998 and 2002 and performing between 1 and 600 procedures per year was recently reported (Cappato, R. et. al, "Worldwide Survey on the Methods, Efficacy, and Safety of Catheter Ablation for Human Atrial Fibrillation," Circulation 2005 Feb 21; 111: 1100-1105). Of the 8745 patients reported to have undergone procedures, 2389 patients (27.3%) required more than one procedure, and 4550 patients (52%) were "asymptomatic without drugs." Remarkably, 524 patients (6%) had at least one major complication. It is important to realize that early experience may have lead to a higher complication rate. On the up side, if this procedure works, you're potentially "cured." It should be noted that doctors will not know if you're cured right away: doctors typically continue warfarin (blood thinner) for three to six months, since it is quite common to have a brief period of atrial fibrillation in the month following the ablation as the heart heals from the procedure. Only after about six months after the procedure do doctors reassess if you can discontinue warfarin. These procedures should be performed in centers performing >100 of these procedures per year by experienced staff to minimize risks. Success rates are also related to the size of the left atrium (larger is harder), associated valvular heart disease (leaky or narrowed heart valves makes this harder ) and long-standing atrial fibrillation makes this tougher. Finally, it is important to remember that to date there remains NO prospective, randomized data showing a SURVIVAL advantage with atrial fibrillation ablation. Therefore, it is REALLY reserved for markedly symptomatic patients, especially those who cannot tolerate the medicine therapy.
A more recent study by Oral et al from the University of Michigan (Oral H, et al. "A Taylored Approach to Catheter Ablation of Paroxysmal Atrial Fibrillation," Circulation 18 Apr 2006; 113: 1824-1831) used a taylored approach to catheter ablation of atrial fibrillation ablation that used a hybrid approach to target different locations in the left atrium thought to be responsible for maintenance of atrial fibrillation. In this study the pulmonary veins were often targetted, but often (69% of patients) a more widespread left atrial ablation pattern was also used that targetted abnormal signals within the left atrium itself (so-called "fractionated electrograms"). This approach had been used by Nademanee et al (Nademanee K, et al, "A New Approach for Catheter Ablation of Atrial Fibrillation: Mapping of the Electrophysiologic Substrate," J Am Coll Cardiol 2004; 43: 2004-2053) in 121 patients with an approximately 80% success rate. Interestingly, Oral et al.'s success rate was similar to other approaches mentioned, with 77% of patients rendered free of atrial fibrillation off drug at 1 year, and a repeat ablation procedure required in 18% to achieve that success rate. With Oral et al's most recent technique, all patients were placed in atrial fibrillation at the procedure outset (if not already in it) and ablation performed until sinus rhythm was restored. 42% of patients in their study never reached this endpoint during the procedure, but in those who did, there was a markedly improved likelihood that sinus rhythm would be maintained long-term. (88% of 88 patients in who atrial fibrillation was rendered non-inducible were free of atrial fibrillation at 11 months, versus 66% of 65 patients who remained in atrial fibrillation during the procedure, p <0.003). Complications, even in this experienced center, occurred in 4 of 153 patients (2%): 2 with transient neurologic events and 2 with cardiac perforation.


Recently, a study on patients with chronic atrial fibrillation (Oral, et. al, "Circumferential Pulmonary-Vein Ablation for Chronic Atrial Fibrillation," New Engl J Med, 2006 March 2; 354: 934-941) was published on a randomized controlled trial comparing circumferential pulmonary-vein ablation compared to amiodarone drug therapy plus two cardioversions in the first three months of therapy. 146 patients were studied of which 77 were assigned to undergo the ablation procedure. Ablation had to be repeated in 20 patients (26 percent) for recurrent atrial fibrillation and in 5 patients (6 percent) for the development of unusual intraatrial reentrant tachycardias (fast circular atrial rhythms), despite this trial being performed in two very experienced laboratories. Regarding the control group, cardioversion (plus amiodarone) was remarkably ineffective at maintaining sinus rhythm with only 3 patients (4 percent) remaining in sinus rhythm after one year. 53 patients in the control group "crossed over" to the ablation arm by one year. While this study confirms success rates of other studies, it is remarkable for several reasons: (1) it suggests chronic atrial fibrillation CAN be approached with catheter ablation techniques in a select cohort of patients, (2) patients did NOT have significant structural heart disease (only 8 percent did) and no patient over 70 years of age was included, (3) all patients received warfarin, and (4) follow-up was limited to 12 months. Despite these limitations, their success rate of 74% (after accounting for the re-do procedures) with only intraatrial reentrant rhythms as their only "complication" was impressive. The issue of improved mortality with catheter ablation was NOT addressed in this study.
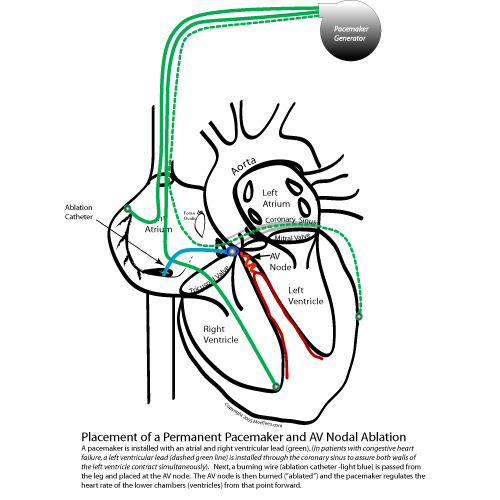
- Implantation of a permanent pacemaker and catheter ablation of the AV node. This procedure is also performed by a cardiac electrophysiologist. Pacemakers prevent too much time between each heart beat. A pacemaker is installed during a minor surgical procedure, typically below the collar bone where doctors can access a vein that leads from one of your arms back to your heart. The pacemaker has two main parts: (1) the wire or wires that course through the vein to the heart chamber(s), and (2) the pacemaker pulse generator (the battery and computer that senses your own heart beat from the wires, and if absent, applies a small electrical impulse to the wires to make the heart muscle contract). As such, this pacemaker system is installed permanently beneath the skin. After the permanent pacemaker is implanted, the electrophysiologist then prepares to destroy the AV node by cauterizing (burning) it using a small temporary wire (called a catheter) which is passed into the heart through a vein from your leg. After the AV node is burned, no impulses from the upper atrial chambers can reach the lower ventricles naturally, and the pacemaker is required to stimulate the lower ventricles to make them contract. This renders you dependent on the pacemaker for the heart to beat, but has a high symptomatic benefit for patients in whom medications have proven ineffective or poorly tolerated ( Kay GN, et al., J Interv Card Electrophysiol; 1998 Jun; 2(2):137-8 and Brignole, et al., Circulation 1997; 96: 2617-2624). Patients with this therapy must remain on warfarin (Coumadin®) since they will no longer perceive their atrial fibrillation.
- Medication - Anticoagulation plus one of two different forms of medications:
- For patients with symptoms of SLOW heart rhythm during atrial fibrillation (such as nearly passing out, passing out, or experiencing intermittent lightheadedness):
- Placement of a permanent pacemaker and anticoagulation - This option is particularly good for patients experiencing periods of lightheadedness when the atrial fibrillation stops and a brief pause in the heart rhythm occurs before the normal rhythm resumes. The pacemaker will prevent the long pause (and hence no blood being pumped to your head) from occuring, since the pacemaker's job is to prevent such long pauses by maintaining a minimum number of heart beats ber minute. While pacemakers are useful devices, they, too have their own set of occasional operative risks involved during their installation (lead dislodgement, infection, cardiac perforation, need for re-operation due to inadequate functioning of the device, etc.) and will require life-long follow-up to assure proper functioning. Nonetheless, these reasons should not preclude this procedure if it is deemed that the symptom-improvement gained by doing the procedure outweighs the risk of doing it.
- Placement of a permanent pacemaker and anticoagulation - This option is particularly good for patients experiencing periods of lightheadedness when the atrial fibrillation stops and a brief pause in the heart rhythm occurs before the normal rhythm resumes. The pacemaker will prevent the long pause (and hence no blood being pumped to your head) from occuring, since the pacemaker's job is to prevent such long pauses by maintaining a minimum number of heart beats ber minute. While pacemakers are useful devices, they, too have their own set of occasional operative risks involved during their installation (lead dislodgement, infection, cardiac perforation, need for re-operation due to inadequate functioning of the device, etc.) and will require life-long follow-up to assure proper functioning. Nonetheless, these reasons should not preclude this procedure if it is deemed that the symptom-improvement gained by doing the procedure outweighs the risk of doing it.
- For patients with NO SYMPTOMS and NO EXCESSIVELY FAST OR SLOW HEART RATE:
- Anticoagulation alone is probably adequate therapy. The AFFIRM trial was the largest randomized, controlled trial of 4060 patients sponsored by the National Heart, Lung, and Blood Institute of the National Institiute of Health, was a very important trial that helped doctors understand that elderly patients over the age of 65 and with no known history of heart valve disease, could live at least as well (or perhaps slightly better with a lower incidence of stroke and death) by just anticoagulating them and NOT trying to restore the rhythm to normal using cardioversion, catheter ablation or medication therapies. It WAS important that patients on anticoagulation with warfarin be carefully maintained at a blood thinning level (also called the "INR" - International Normalized Ratio) of two to three (patients with artificial heart valves should have slightly higher values of 2.5-3.5). What does this INR mean when it's 2-3? It means it takes 2-3 times the amount of time to clot your blood as a normal control. INR levels over 4.0 are associated with a significantly increased risk of bleeding.
- Anticoagulation alone is probably adequate therapy. The AFFIRM trial was the largest randomized, controlled trial of 4060 patients sponsored by the National Heart, Lung, and Blood Institute of the National Institiute of Health, was a very important trial that helped doctors understand that elderly patients over the age of 65 and with no known history of heart valve disease, could live at least as well (or perhaps slightly better with a lower incidence of stroke and death) by just anticoagulating them and NOT trying to restore the rhythm to normal using cardioversion, catheter ablation or medication therapies. It WAS important that patients on anticoagulation with warfarin be carefully maintained at a blood thinning level (also called the "INR" - International Normalized Ratio) of two to three (patients with artificial heart valves should have slightly higher values of 2.5-3.5). What does this INR mean when it's 2-3? It means it takes 2-3 times the amount of time to clot your blood as a normal control. INR levels over 4.0 are associated with a significantly increased risk of bleeding.
What About Freezing Therapy (Cryoablation) for Atrial Fibrillation?
Freezing therapy or "cryoablation" uses a catheter that can freeze tissues to -70 degrees Celsius, rather that burn tissue by resistive heating (as is performed by radiofrequency energy). Freezing to only -30 degrees Celsius fails to create identifiable damage to the tissues. There are significant differences in the application of therapy delivered by cryoablation compared to radiofrequency energy. First of all, each lesion created by cryoablation takes at least four minutes per lesion (radiofrequency works in 30-60 seconds, typically). Secondly, cryoablation is thought to be safe to apply to the pulmonary vein because of reduced risk of serious scar formation, and hence a lower incidence of pulmonary vein stenosis (narrowing). Also, application of cryotherapy is painless compared to radiofrequency energy which sometimes feels like "heartburn" when it is applied. These advantages have been offset by prolonged procedure times with pulmonary vein isolation. One study demonstrated that it took 65+/-39 minutes per pulmonary vein to perform isolation and an average procedure time of 4-5 hours (290+/-101 minutes) (Wong T, et al., "Percutaneous Pulmonary Vein Cryoablation to Treat Atrial Fibrillation," J Interven Cardiac Electrophys, 2004; 11: 117-126)
To date, cryoablation has been tried with limited success (and no large trials) in catheter-based pulmonary vein isolation procedures, and its results have NOT been as favorable as radiofrequency energy. This has been because full-thickness lesions near the pulmonary vein openings compared to radiofrequency energy have been challenging to achieve. In part this may be due to the high blood-flow velocities which maintain tissue temperatures and make cooling more challenging. Therefore, there has been an attempt to make a circular catheter that can encircle the pulmonary vein and achieve full-thickness lesions effect in fewer freezing applications, but the catheter quality and difficulty identifying precise anatomic catheter positioning has made isolation difficult with a single catheter type. More recently, trials with a cryo-balloon catheter that fits within the pulmonary vein opening are underway, but it remains undertain how effective this therapy will be.
In summary, work continues with catheter-based cryoablative therapy, but its application to atrial fibrillation ablation has been limited and long-term efficacy poorer than radiofrequency-applied therapy to date.
There may be a role for adjunctive cryotherapy during open-chest surgical procedures, however. Surgeons have long used cryoablation in the operating room during open-heart surgery, and cryoablation is still used during some open-chest/open-heart procedures during the Maze procedure to apply lesions near the heart valves. Cryoablation is unique in its inability to cause damage to the coronary arteries (which lie in close proximity to the tricuspid and mitral valves) during the ablation procedure.
My Doctor Says I have Atrial Flutter, not Atrial Fibrillation. How is Atrial Flutter Different From Atrial Fibrillation?
- Atrial flutter is also a atrial rhythm disorder, but unlike atrial fibrillation which has multiple wavelets circulating within the atria simultaneously, atrial flutter has only one wavelet of a loop-the-loop rhythm that circulates within the atria. Typically, this wavelet of electricity circulates 240-280 times per minute in the right atrium around the tricuspid valve (the valve between the right atrium and right ventricle). Only rarely does this rhythm occur within the left atrium. This is because the right atrium is structurally slightly different from the left atrium and contains a ridge of tissue along its side edge that acts to direct the electricity around the border to the tricuspid valve. Now the ventricles are often driven at rates slightly slower than the atria because the AV node prevents all of the impulses from stimulating the ventricles too fast. However, if every other electrical beat is conducted to the ventricles, the heart can still beat at the relatively fast rate of 130-150 beats per minute and might continue this fast even while resting in some patients. The good news about this rhythm as opposed to atrial fibrillation, is that this rhythm is very successfully treated with catheter ablation.
- Catheter ablation for atrial flutter: Originally described in 1992 (Feld GK, et al., Circulation 1992; 86: 1233-1240), it is a highly effective, relatively safe procedure with a proven track record. Catheter ablation of atrial flutter is a much less risky procedure than catheter ablation for atrial fibrillation because to can be performed with the right atrium. Because of this, there is almost no stroke risk, since the right atrium and right ventricle only pump blood to the lungs and not the head or body. Therefore, if a clot were to form of the burning wire, it would be unlikely it could ever cause a stroke. To perform an atrial flutter ablation, the cardiac electrophysiologist burns a small line from the tricuspid valve to the vein on the back floor of the right atrium where the large vein (the inferior vena cava) enters the right atrium by using a flexible and steerable special ablation (burning) wire. The electrical wavefront that circulates around the tricuspid valve in atrial flutter then will collide with the burned "line" connecting the valve to the vein, and stops the loop-the-loop rhythm of atrial flutter. It is fairly easy for the electrophysiologist to test to be sure that no conduction occurs across this line after interrupting the rhythm, thereby limiting the recurrence rate of atrial flutter late after the catheter ablation procedure. Overall success rates with this procedure are about 95% and we perform these usually as "same-day" surgical procedures. Because patients occasionally develop atrial fibrillation after an atrial flutter catheter ablation procedure, it is our practice to continue anticoagulation for at least 6 months after the procedure.
- Pacemaker to treat atrial flutter - Although used infrequently, there are now pacemakers that can be installed (with one wire in the atrium and one wire in the ventricle) that can detect when the atrium develops a rapid rhythm and attempt to pace the heart back into normal rhythm. While these pacemakers exist, they do not cure atrial flutter and are not as effective as catheter ablation at controlling this rhythm. Therefore we rarely use these devices.
Where Can I Get More Information?
- Other good sources about atrial fibrillation and atrial flutter include:
- Heart Rhythm Society - An international society dedicated to the treatment of heart rhythm disorders.
- Aboutatrialfibrillation.com - A website sponsored by St. Jude Medical, Inc. that reviews the basics of atrial fibrillation and the therpies available.
- AFFacts.org - The Atrial Fibrillation Foundation website. A good overall reference, but a bit outdated.
- Support Groups:
- Yahoo support group: http://health.groups.yahoo.com/group/AFIBsupport/
- MedTees.com's support forum - A cardiac electrophysiologist and psychologist team to provide support for patients with difficult diseases.
- And of course, web search engines such as Google or Yahoo also can connect you with other sites or institutions treating atrial fibrillation.
CONCLUSIONS
Hopefully this tutorial has helped clarify your rhythm disorder and shed light of how your doctor may have selected a particular form of therapy for your atrial fibrillation. Remember several important "absolutes:" (1) anticoagulation is very important to reduce stroke and (2) symptoms often guide your doctor's therapeutic recommendation(s). So be sure to share with your doctor how the atrial fibrillation makes you feel. If your are already under one form of therapy for atrial fibrillation, remember to tell your doctor about side effects you might be experiencing from medications or if your symptoms don't improve with a particular therapy, since many therapies are available for the treatment of atrial fibrillation.
Find this helpful? Contemplating a catheter ablation procedure? Check out MedTees.com, a site devoted to chronic disease awareness and the support of patients with difficult diseases by contributing to various research and charitable organizations. There you can join discussions with other patients in our Forums and find out other information in our Tutorials section.
