(Requires Adobe Acrobat Reader)
Catheter Ablation for Supraventricular Tachycardias
- A Patient's Guide -
Westby G. Fisher, MD, FACC
Director, Cardiac Electrophysiology
Evanston Northwesten Healthcare
Evanston, IL, USA
(Last Updated 14 May 2006)
AV Nodal Reentrant Tachycardia (AVNRT)
Introduction
By far the most common supraventricular tachycardia in adults, AV nodal reentrant tachycardia is also one of the most easily cured rhythms encountered by the heart rhythm specialist (cardiac electrophysiologist). This is not to say that all patients must undergo an invasive procedure (called an "electrophysiology study with catheter ablation") or that all procedures, themselves, are "easy." But relatively speaking, many patients do well with catheter ablation. Patients who have self-limited and infrequent episodes that are easily managed with medications and do not necessarily have to undergo this procedure. Nonetheless, for highly symptomatic patients, catheter ablation is now considered the therapy of choice for treatment of this disorder.
Where is the AV node?
The AV node lies between the upper chambers of the heart (the atria) and the lower chambers of the heart, the ventricles. The AV node's normal job in your heart is two-fold: (1) to permit the electrical impulse arising in the atrium to pass to the ventricles and (2) to delay the electrical impulse slightly to allow time for blood to physically move from the atria to the ventricles.
What Does Tachycardia Mean?
Tachycardia is a medical term that means, literally, "fast" (tachy-) "heart" (-cardia). In adults, tachycardia is usually defined as heart rates above 100, but patients with AV nodal reentrant tachycardia typically have heart rates from 150-200 beats per minute. Babies normal heart rates can be as high as 130-150 beats per minute, and their heart rates during periods of AV nodal reentrant tachycardia can be correspondingly faster. When the attacks of rapid heart rhythm are intermittent, the medical term for this is "paroxysmal." Since AV nodal reentrant tachycardia is one form of supraventricular tachycardia that occurs intermittently, it is often referred to as "paroxysmal supraventricular tachycardia," or PSVT. However there are other mechanisms for PSVT, including SVT's caused by the presence of a small muscle fiber that makes an extra connection between the atrium and ventricles besides the AV node called an "accessory pathway." Babies and young children are usually more likely to have an accessory pathway, than are adults, but they can exist in either population. For this reason, before a curative procedure is performed, doctors must first determine which form of PSVT exists. An electrophysiology study (a heart electrical study) confirms which type of PSVT exists so that appropriate therapy can be administered.
Why is this rhythm "re-entrant?"
A reentrant rhythm is one that circulates in a circular pattern. If the circuit for the abnormal heart rhythm lies between the atria and ventricles (as in the case of the AV node), then a reentrant rhythm would circulate from the atrium to the ventricles, then back to the atrium, then back to the ventricles, and so on. (A rhythm can still be reentrant if it is confined to one chamber: in the case of atrial flutter, the rhythm circulates within the atrium just above and around the tricuspid valve at a rapid rate.) In the case of AV nodal reentrant tachycardia, the way the electricity circulates between the atria and ventricles in a circular pattern is because there are two halves of the AV node that have differing conduction properties. One pathway conducts the electrical impulses faster and the other conducts them more slowly from the top (atria) to bottom chambers (ventricles).
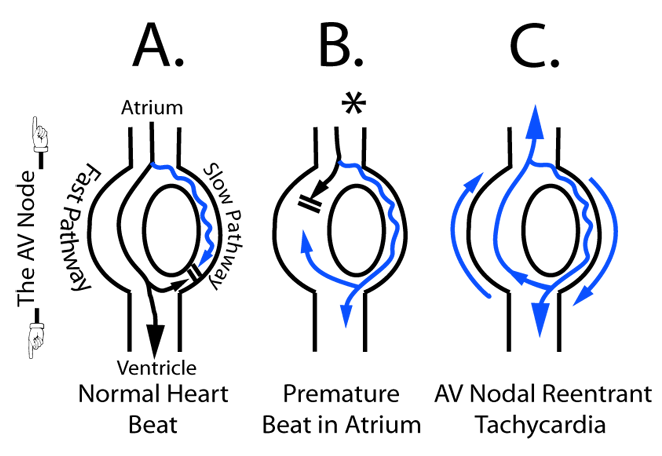
In the normal heartbeat, the impulse travels from the atrium to ventricles primarily down the AV nodal "fast pathway" (black line, Panel A above) and tries to go down the slower conducting pathway as well (blue line, Panel A), but collides with the impulse form the fast pathway that reaches the far end of the slow pathway first, causing normal conduction from the top to bottom chambers.
To initiate the tachycardia, a premature beat occurs outside the AV node (denoted by the asterisk, Panel B above). In this case, the early beat is prevented from traveling down the faster pathway because of its prematurity, but the slower conducting properties of the slow pathway allow this premature beat to pass to the lower portion of the AV node. When the impulse reaches this lower portion of the AV node, the electricity passes to the ventricles but also passes back to the atrium via the now-functioning fast pathway. After going back to the atrium, the electricity can pass back down the slow pathway again to sustain the reentrant rhythm. The beat can then conduct back up to the atrium using the fast pathway (upward blue line, Panel C), and then reenter down the slow pathway (downward blue line, Panel C), creating the AV nodal reentrant tachycardia.
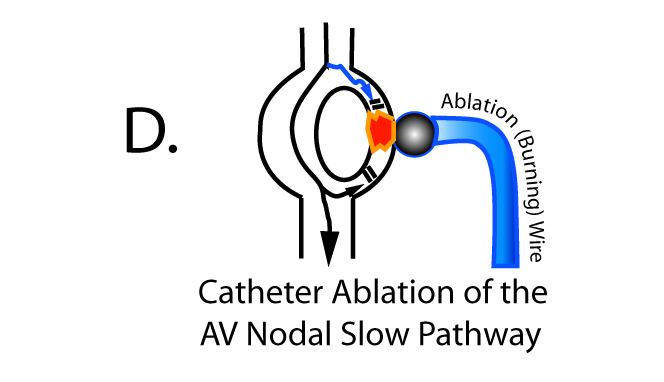
This loop-the-loop rhythm continues until it is interrupted by (1) nerve inputs to the AV node that can slow conduction to the point where it stops, (2) medications that slow or stop conduction through all or a portion of the AV node, (3) and electrical shock (called cardioversion) that resets the heart, or (4) physically burning or cauterizing one of the two halves of the AV node to stop conduction ("catheter ablation") - The ablation (burning) of the AV nodal slow pathway is the definitive curative procedure for this disorder: Panel D below:
Why Me?
Another common question posed is "Why Me?." Be reassured that most people probably have the anatomy, but not necessarily the physical conduction properties, of the two halves of the AV node to develop the rapid heart rhythm. MOST people have completely normal structure and function of their heart. Therefore, the presence of this rhythm does not necessarily mean that there is anything structurally wrong with your heart.
Why Now?
What is unusual about AV nodal reentry is that is often manifests later in life for many people. Why this is can potentially be explained by the change of conduction properties of the two halves of the AV node (the "slow" and "fast" pathways). The change in conduction properties of one of the pathways relative to the other pathway may account for enough difference in the conduction speed through the two pathways that reentry can be sustained. In earlier years, if both pathways conducted quickly and at about the same conduction speed, then the two pathways would have performed as though they were one large pathway from top to bottom chamber and reentry would not be possible.
What Therapies Exist?
As mentioned above, catheter ablation is now considered the therapy of choice in symptomatic patients with supraventricular tachycardias, including AV nodal reentrant tachycardia. This does not mean that all patients MUST undergo the procedure, but if catheter ablation is successful, you are effectively "cured" of the rapid heart rhythm caused by this disorder. Alternatives to catheter ablation are outlined below.
Alternative therapies include medical therapy with a beta blocker medication (like propranolol (Inderal®), atenolol (Tenormin®), metoprolol (Lopressor®), etc. Beta blocker medications lower adrenaline levels and prevent the rhythm from occurring and slow the rhythm if it does recur.
Alternatively, calcium channel blockers are also often prescribed an act to slow conduction through the AV node, thereby preventing reentry as well. These include diltiazem (Cardizem®), or verapamil (Calan®). Thes drugs are usually taken continuously, but can also be used on an "as needed" basis if tachcardia episodes are infrequent.
Other drugs like digoxin have been used, but are not as effective. Antiarrhythmic drugs such as Amiodarone (Pacerone®) and sotalol, can be used as well, but generally have more potential dangerous long-term side effects, and must be monitored closely.
Finally, some folks have recurrent rapid rhythms are infrequent and easy to self-control by using various methods to increase neural slowing to the AV node (so-called, "vagal maneuvers"). Using these maneuvers, one can sometimes stop the arrhythmia. These maneuvers include:
- Bearing down forcefully like you're having a bowel movement for 5-10 seconds, then slowly exhaling.
- Rubbing the carotid artery in the neck while lying down for approximately 5 seconds
- Placing very cold (soaked in ICE water) cloth on the face abruptly.
- Coughing forcefully
If one of the maneuvers is effective and the rhythm occurs infrequently (e.g., once a year) or is self-limited, then further therapy might not be required.
If these maneuvers are ineffective and you are symptomatic, you should go to an emergency room. Doctors there usually use a very short acting medication called "adenosine" to correct the rhythm. This medication is injected rapidly in your vein though an IV and one feels a very uneasy, warm sensation that passes quickly (usually in seconds) and the arrhythmia usually will stop. On rare occasions the adenosine may not work at low doses, and higher doses are needed. (Transplant patients are the exception, these patients usually need one tenth of the usual dose of adenosine, since they are VERY sensitive to the heart rate slowing effects of this drug on their transplanted heart.)
How is Catheter Ablation Performed?
First of all, you'll be asked to eat NOTHING after midnight the evening before the procedure. Not uncommonly, your doctor might ask you to also NOT take some of the heart rhythm medications before the procedure so your rhythm can be initiated easier during the electrophysiology study (heart electrical study).
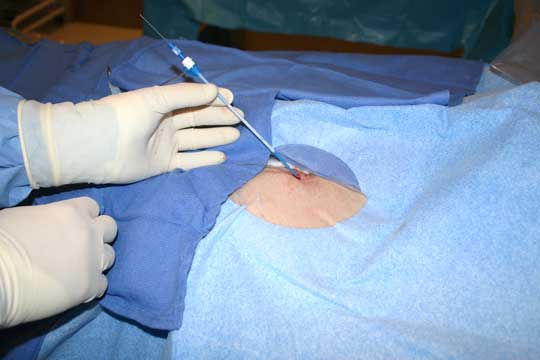
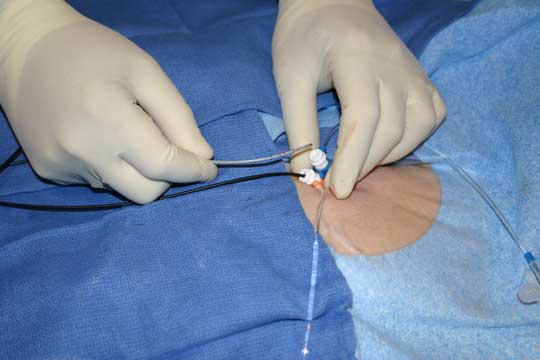
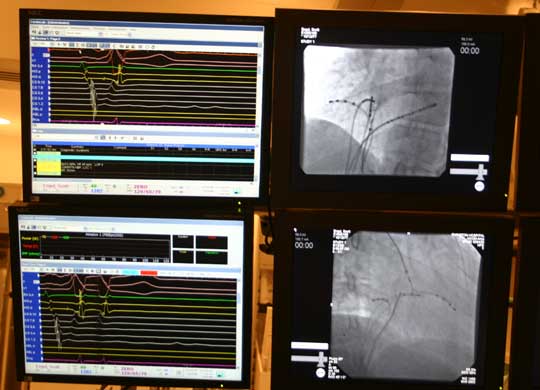
You will first to to a pre-procedure holding area, where and IV will be started and blood taken for analysis to assure the procedure is performed safely. Women of reproductive age commonly have pregnancy test the morning of or the day before the procedure. Next you will be connected to a series of EKG leads and a large patch electrode on your back and chest (these serve two purposes: (1) to apply energy to your heart during the "ablation" procedure, and (2) to shock the heart back to normal rhythm in the rare event an irregular or dangerous rhythm were started during the testing of your heart.) The leg area near the groin will be cleaned, possibly shaved, and prepared for the procedure. You will then be transported into the electrophysiology laboratory and asked to lie on a thin table under an xray tube. You'll be secured to the table gently. The legs will again be prepped and a large drape placed over your chest and legs. You will be sedated with medications that help relieve anxiety and discomfort during the procedure. The doctor will then use a local anesthetic to numb the legs at the crease where your leg attaches to the pelvis near the groin. After this, a small needle will be painlessly placed into the vein of your right and left legs and a series of small tubes placed in the veins that have one-way valves on them to permit the passage of wires, but no bleeding from your leg.(Figure 1 below) A series of wires are then passed to your heart under xray guidance. (Figures 2 and 3 below) There are no nerves inside the blood vessels leading to your heart, so this is typically completely painless. Once in the proper place, your doctor will measure conduction times within the heart, and then pace the heart in the upper and lower chambers to study the conduction properties of the heart chambers. Skipped heart beats will be applied using a special computer and attempts will be made to induce the abnormal heart rhythm you have been experiencing. You may be able to perceive heart skipping or racing as this portion of the testing is performed. Occasionally, an adrenaline-like medication is required to start the heart rhythm. When this medication is administered, you also might notice your heart pounding more than usual. Do not be concerned, stopping the infusion of this medication will stop the pounding sensation in about 15-20 minutes.
Once the heart rhythm is started, the doctors will study what it takes to initiate and terminate the rhythm. After this is performed, preparations are made to perform catheter ablation. A special steerable wire with a slightly enlarged tip is passed from the legs to the heart and positioned to the critical portion of the conduction pathway required to sustain the rhythm (this is determined during the earlier pacing studies). One or more applications of radiofrequency energy (the name "radiofrequency" comes from the fact that it is a 500kHz alternating current electricity that is applied, and happens to be at the same frequency as 500 on your AM radio dial!). This alternating current passed from the patch on your back, through your body, and received at the ablation wire in your heart. This causes the tip of that wire to become hot (like the filament of a lightbulb) and cauterizes (burns) the tissue beneath the wire. If placed correctly, this should interrupt the reentrant circuit and no further rapid heart beats occur.
After the ablation procedure, additional skipped beats are applied to the heart to be sure no further heart rhythms occur. Once the doctor is satisfied that no abnormal rhythms can occur, you are often monitored in the lab an additional 15-30 minutes and repeat testing performed one moe time. If the abnormal heart rhythms STILL cannot be re-initiated, then the procedure is considered complete. All catheters (wires) will be removed from your heart, the small tubes placed in your legs will be removed, pressure will be applied to the areas of the catheters, then band-aides applied over the wounds. You'll then be removed from the laboratory and observed for at least 4 hours to assure you have tolerated the procedure well.
What Are the Risks With Catheter Ablation?
The greatest risk with catheter ablation of a portion of the AV node, is that of developing "complete heart block." That is, is the ablation (burning) catheter burns BOTH the fast and slow pathways of the AV node, then NO impulses can travel from the atrium to ventricle, rendering the patient pacemaker-dependent (that is, a permanent pacemaker would have to be installed). The risk of development of this complication is less than or equal to 1 percent. Other risks include, but may not be limited to, bleeding (especially at the sites where the catheters enter the leg bleed vessels), development of a communication between the vein and artery of the leg (called a "fistula") that has to be surgically corrected, development of a large blood clot in the veins of the legs (called a "deep venous thrombosis or DVT), damage to the heart itself, including perforation of the heart requiring emergent drainage of blood from the lining around the heart (called the pericardium), stroke, infection, nerve injury to the leg nerve, and a reaction to the medications or contrast agents that might be used during the procedure. On occasion, some electrophysiologists place a catheter in the vein in the upper chest area just beneath the collar bone to go to the heart. It is possible to inadvertently puncture the lung while placing that catheter (called a "pneumothorax"). Radiation (xray) or electrically-induced skin damage can also occur. In total, collective risks in experienced centers are less than or equal to approximately 1.5%. Death is an extremely rare complication.
What Happens After the Catheter Ablation
If your procedure is uncomplicated, most people return home in 4-6 hours. Your doctor will often stop at least some of your heart rhythm medications after the procedure. Have a family member or friend drive you home from the hospital, and normal activities should be able to resume in one to two days after the procedure. Heavy exertion should resume only after the leg sites have completely healed. It is common to feel a small bump or note a small bruise at the sites where to catheters were inserted into the legs. These usually completely resolve within a few weeks.
When Should I Call the Doctor After My Procedure?
Call your doctor if:
- The catheterization sites in your legs begins to bleed or the site becomes increasingly painful or swollen
- You feel shortness of breath or chest discomfort
- You have a fever over 100.5
- You feel the symptoms of your heart rhythm problem return
Where can I get additional information?
Additional information can be found at the Heart Rhythm Societies Public and Patients Webpage at: http://www.hrspatients.org/.
Or you can post a question on the MedTees.com Forum section.